Episodes

Tuesday Jun 03, 2025
Intensity
Tuesday Jun 03, 2025
Tuesday Jun 03, 2025
Intensity is a crucial concept in ultrasound physics, particularly for understanding image quality and patient safety.
Here's what you need to know about intensity:
- Definition and Units: Intensity describes the energy density within a sound beam. Its units are watts per square centimeter (W/cm²).
- Calculation: Intensity is calculated as beam power divided by the cross-sectional area.
- Intensity (W/cm²) = Power (W) / Beam Area (cm²).
- Determinants and Adjustability: Intensity depends on the source specifications and can be adjusted by the operator.
- Behavior in Tissue: As sound propagates through tissue, both intensity and power diminish. This reduction in intensity is part of the overall attenuation of the sound wave.
- Safety and Bioeffects: Intensity is a key metric for evaluating safety and bioeffects. Standard imaging intensities in ultrasound are generally considered safe, with no known bioeffects. However, ultrasound can potentially cause thermal and mechanical effects, and the thermal effect arises from temperature increases due to ultrasound waves being absorbed by biological tissues.
- Relationship with Duty Factor: The duty factor represents the proportion of time a pulse is actively propagating and is important for quantifying intensities. Clinical duty factors are typically low (0.001-0.01), as listening intervals dominate to permit echo reception. Low duty cycles, combined with short pulse lengths, ensure that only one pulse traverses the imaging plane at a time, localizing energy deposition spatially and temporally, which helps improve safety. Understanding duty factor principles aids in evaluating potential bioeffects.
- Relationship to Output Power and Image Brightness: Transducer output (also known as acoustic power, pulser power, or transmitter output) directly influences the brightness level across the entire ultrasound image and is regulated by the excitation voltage from the pulser. Adjusting transducer output upwards can improve the signal-to-noise ratio, enhancing image clarity. However, increasing transducer output also increases patient exposure to ultrasound. The ALARA (As Low As Reasonably Achievable) Principle guides these adjustments, prioritizing minimizing patient exposure by first adjusting receiver gain to optimize image brightness before increasing output power.
Tuesday Jun 03, 2025
Specular Reflection
Tuesday Jun 03, 2025
Tuesday Jun 03, 2025
Specular reflection is a fundamental phenomenon in ultrasound imaging that you need to understand:
- Definition: Specular reflection occurs when ultrasound energy strikes a very smooth surface and bounces back to the transducer, similar to how light reflects off a mirror. This bouncing back of sound energy is critical for creating the image displayed on the ultrasound monitor.
- Conditions for Occurrence: This type of reflection is most pronounced when the wavelength of the sound wave is considerably smaller than the irregularities of the reflecting boundary.
- Importance of Angle: The visibility of specular reflectors heavily depends on the angle at which the ultrasound wave strikes the reflector, known as the angle of incidence. Specular reflectors are most clearly visible when the ultrasound wave hits the reflector perpendicularly (at a 90° angle). If the angle deviates from this perpendicular incidence, the visibility of these reflectors significantly diminishes because the reflected sound waves are not directed back towards the transducer.
- Contrast with Non-Specular/Diffuse Reflection: Unlike specular reflection, which involves organized reflection from smooth surfaces, non-specular or diffuse reflection occurs when sound waves strike rough or irregular surfaces, causing the reflected sound to scatter in various directions. Diffuse reflection provides a more detailed and textured image of internal structures, especially those with uneven surfaces, as it involves the scattering of sound waves in multiple, random directions.

Tuesday Jun 03, 2025
Artifacts
Tuesday Jun 03, 2025
Tuesday Jun 03, 2025
In ultrasound imaging, artifacts are important to understand as they can affect the accuracy of diagnosis and treatment.
Here's what you need to know about artifacts:
- Definition and Types: Artifacts are distortions or inaccuracies in the ultrasound image. Common types of artifacts include:
- Reverberation
- Shadowing
- Refraction artifacts
- Importance of Recognition and Correction: It is crucial to recognize and correct these artifacts to ensure accurate diagnosis and treatment.
- Doppler Artifacts: These are a specific type of artifact related to Doppler ultrasound.
- Cause: Doppler systems transform frequency shifts, usually from moving red blood cells, into colors and spectra. However, low-velocity motion, such as pulsating vessel walls, can create minor Doppler shifts that appear as artifacts.
- Examples: Common Doppler artifacts include color flash or ghosting.
- Correction/Mitigation:
- Wall filters (high-pass filters) are used to help eliminate these low-magnitude shifts, thereby reducing artifacts like color flash or ghosting.
- It is important to note that simply reducing color Doppler gain will not fix ghosting artifacts because it removes reflections from tissues before it removes reflections from blood cells.
Monday Jun 02, 2025
Duty Factor
Monday Jun 02, 2025
Monday Jun 02, 2025
The duty factor is a significant parameter in ultrasound imaging, particularly concerning the characteristics of the emitted pulse and patient safety.
Here's what you need to know about duty factor:
- Definition: The duty factor represents the proportion or percentage of time that an ultrasound pulse is actively propagating. It can be expressed as a percentage or a fraction ranging from 0% to 100%.
- Continuous Wave vs. Pulsed Operation: A 100% continuous duty cycle corresponds to continuous wave emission, while 0% defines a quiescent system. However, imaging inherently utilizes pulsed ultrasound with fractional duty factors below 100%, typically around 0.01 or less clinically.
- Typical Clinical Values: Clinical duty factors typically range from 0.001 to 0.01. This means that the system is listening for echoes for most of the time, allowing for echo reception from depths up to 30 cm.
- Determinants and Adjustability: The duty factor depends on adjustable timing circuit parameters and is determined by the sound source. While it's primarily source-dependent, the sonographer's adjustments to imaging depth can indirectly change the duty factor, influencing image quality and depth.
- Relationship to Safety: Low duty cycles, combined with short pulse lengths, are crucial for safety. This pulsing approach ensures that only one pulse traverses the imaging plane at a time, localizing energy deposition spatially and temporally, thereby improving safety. Understanding duty factor principles helps in evaluating potential bioeffects.
- Impact on Intensity: The duty factor is important for quantifying intensities.

Monday Jun 02, 2025

Monday Jun 02, 2025

Monday Jun 02, 2025
Tuesday Feb 18, 2025
Tuesday Feb 18, 2025

Thursday Feb 13, 2025
Thursday Feb 13, 2025
Thursday Feb 13, 2025

Thursday Feb 13, 2025
Tuesday Feb 11, 2025

Tuesday Feb 11, 2025
Understanding Image Processing: Pre vs. Post
Tuesday Feb 11, 2025
Tuesday Feb 11, 2025
In this episode, we explore the fascinating world of image manipulation, focusing on the critical differences between pre-processing and post-processing techniques. Discover how pre-processing enhances image quality by compensating for sound wave attenuation and improving uniform brightness. Learn about the irreversible nature of pre-processing and how it adjusts grayscale values to match human perception.
Additionally, we delve into post-processing, where changes can be undone, increasing the versatility of displayed images. Understand how post-processing magnifies specific areas for better visualization and creates three-dimensional images from two-dimensional ones. The episode highlights the timing and impact of each method on image quality, providing a comprehensive overview for enthusiasts and professionals alike.

Tuesday Feb 11, 2025
Constructive Interference
Tuesday Feb 11, 2025
Tuesday Feb 11, 2025
Dive into the fascinating world of physics as we explore what happens when two kids jump on a trampoline at the same time. Discover the concept of constructive interference and how synchronizing their jumps creates a thrilling increase in energy and momentum.
In this episode, we use a simple trampoline to illustrate complex energy dynamics, making science accessible and fun for listeners of all ages.

Tuesday Feb 11, 2025
Destructive Interference
Tuesday Feb 11, 2025
Tuesday Feb 11, 2025
In this intriguing episode, we delve into the fascinating phenomenon of destructive interference in music. Discover how two sound waves can meet and cancel each other out, resulting in quieter or even silent spots within a musical piece. Explore the science behind this sound wave interaction and its effects on audio perception.
We unravel how destructive interference not only weakens sound waves but can also create gaps or darker spots in auditory imagery. Join us as we examine the intricacies of this acoustic occurrence and its implications for the creation and experience of music.

Thursday Feb 06, 2025
Accoustic Impedence
Thursday Feb 06, 2025
Thursday Feb 06, 2025
In this episode, we explore the intriguing dynamics of moving a heavy swing, drawing parallels with the rhythmic flow of music. Dive into the challenge of building momentum and discover the surprising connection between physical force and sound. Join us as we uncover the hidden harmony that powers both the push of a swing and the pulse of a melody.
Thursday Feb 06, 2025
Arrows
Thursday Feb 06, 2025
Thursday Feb 06, 2025
In this gripping episode, we delve into the unique perspective of an ultrasound machine during a high-stakes medical emergency. The narrative unfolds as the machine witnesses a code blue response, capturing the tense moments from the first sign of cardiac arrest to the eventual revival of the patient's heartbeat. Experience the chaos, the hope, and the triumph as the medical team fights to restore life, all through the steady gaze of technology dedicated to saving lives.
Tuesday Feb 04, 2025
Exploring the Different Types of Doppler Ultrasound
Tuesday Feb 04, 2025
Tuesday Feb 04, 2025
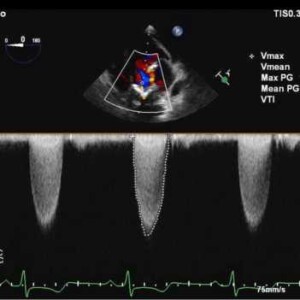
In this episode, we delve into the fascinating world of Doppler ultrasound, focusing on the different types available today. Our discussion primarily highlights Pulsed Wave Doppler, a technique known for its range resolution capabilities. We explore its unique features and applications in the medical field, making complex concepts easy to understand.

Sunday Feb 02, 2025
Doppler and Duplex Imaging ( Commercial Free)
Sunday Feb 02, 2025
Sunday Feb 02, 2025
Ever wish you could see your blood flowing in real-time? Doppler ultrasound technology makes that possible, allowing us to delve deep into the intricacies of blood flow with techniques like continuous wave, pulsed wave, and color flow Doppler. This episode unpacks the science behind how Doppler ultrasound works, from measuring the speed and direction of blood flow to revealing the dynamic images often seen in medical shows.
Imagine an ambulance's siren changing pitch as it passes by; that's the Doppler effect, applied to visualize blood flow inside the body. Our journey unravels various Doppler techniques, uncovering their unique strengths, quirks, and real-world applications in medical imaging.
Venturing into duplex imaging, we explore how combining Doppler with real-time anatomical imaging provides an even more comprehensive view of blood flow and vessel structure, enhancing diagnostics in specialties like cardiology and vascular imaging.
As we look to the future, advancements like contrast-enhanced ultrasound and elastography promise to revolutionize the way we detect and diagnose with sound waves, showcasing the potential of Doppler ultrasound as an invaluable tool across medicine.